Gut-Brain Parkinson’s Bi-directional Connections
Gut-Brain Parkinson’s Bi-directional Connections
Parkinson’s Disease
Role of Naturopathic Medicine in Parkinson’s Disease Management
There are several theories about why Parkinson’s disease is on the rise: ongoing environmental chemical exposures, head traumas, high levels of diabetes, reduced smoking levels and other lifestyle factors. From my naturopathic medical perspective, I look at a range of other factors and treatments that may provide a broader approach as summarized below.
Role of the digestive / intestinal function in Parkinson’s Disease
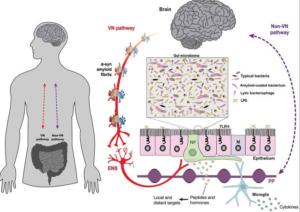
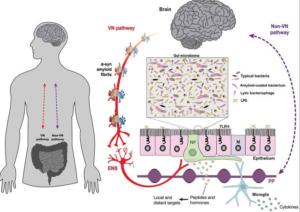
One of the newest relationships discovered in Parkinson’s research is that the cell/molecular signs of Parkinson’s activity (the level of alpha-synuclein in affected nerves) may begin in the nerves of the digestive system before it appears in the nerves of the brain. This makes sense considering a common early sign of Parkinson’s disease (PD) is poor intestinal function (eg: constipation and poor stomach function). It has also been found that people with PD have a different makeup of microbes in their digestive tract; they have more ‘pro-inflammatory’ bacteria that may be a trigger for the neuro-inflammation typical in patients with PD. See the image here of the two-way flow of information between the intestinal lining and the brain (note, flow can be through nerves, lymphatic and blood vessels – Image: Santos et al 2019). Dysfunctional digestion may also have a role in how some antiparkinsonian drugs are absorbed; for instance, small intestinal bacterial overgrowth and Helicobacter pylori infection affect intestinal muscle function by interfering with the absorption of anti-parkinsonian drugs.
Recent studies have also found that many people with PD have differences in the integrity of the intestinal barrier, often referred to as ‘leaky gut.’ One theory is that such changes in intestinal structure may allow intestinal debris or intestinal microorganism to enter or trigger the development of neurological changes – according to the Braak theory.
Treatment of those with Parkinson’s disease and possibly parkinsonism in general must at some level involve the digestive system. More detailed naturopathic testing of the digestive system is appropriate and may include testing for several markers of digestion, intestinal barrier function (blood/urine/stool test) and to examine the spectrum of microorganisms present in the digestive tract.
Role of nutrition in Parkinson’s Disease
Vitamin D. Once in the body, vitamin D converts to having a significant hormonal-type role in the body, including the brain. Recent review studies have concluded that vitamin D is lower in those with PD and that some people with PD can actually delay progression of their disease. I have found it useful to test and treat and retest vitamin D to make sure it is in a healthy part of the normal range. It is very important to retest vitamin D since it is not always easily absorbed; note that these patients often already have digestive problems.
Amino acids. Several amino acids (building blocks of important functional proteins in the brain) may be beneficial in those with PD. Cysteine may help with regulating dopamine and improving symptoms. Tryptophan may help in the production of important neurohormones. Threonine may help with spasticity. Taurine may help with the motor symptoms of PD. Early laboratory studies have shown that taurine has several benefits: protects brain cells from the damage from neurotoxins, promotes brain cell development, helps support mitochondria and even muscle function. Carnitine is a mitochondrial neuroprotectant which may have a role in the proper transport of dopamine. Note that protein can also affect the absorption of levodopa/carbidopa, so dietary protein or supplemental protein intake may need to be separated from these medications.
Other nutrients. B-vitamins, selenium, zinc, magnesium and several others may be important in overall cognitive and motor functioning and is reasonable to test.
Relationship of digestive function and nutrition. One of the problems with nutrition in those with PD is that their improper digestion may reduce the effectiveness of any treatment, whether pharmaceutical or nutritional or herbal…any oral treatment. Future treatments may require novel ways of administering treatment to provide a more consistent benefit. One of the treatment options I provide is intravenous nutritional treatment – this is utilized based on an individual naturopathic assessment and may not be necessary for every patient.
Role of toxicity in Parkinson’s Disease
Several toxins have been implicated in PD: pesticides, lead, aluminum, cadmium, mercury, MPTP. It is challenging to connect any chemical and causation, though these chemicals are known neurotoxins. Part of the naturopathic assessment involves screening for several toxins. Eliminating the source is suggested as well as removing such chemicals from the body may be important. “Glutathione” is a nutrient that the body produces, made up of three amino acids. Glutathione is known to protect the nerves, can help detoxify neurotoxins and is commonly deficient in those with Parkinson’s Disease. It has been found to symptomatically improve those with Parkinson’s Disease, more likely in the early to moderate stages.
Naturopathic treatment of Parkinson’s Disease and Parkinsonism
The naturopathic approach to those with Parkinson’s disease is a process that involves a thorough evaluation of your health history, examination and testing to develop individualized treatment. The actual treatment may be staged and can include a variety of methods including optimized nutrition (oral and by injection), improving digestion, resolving toxicity, targeted balance exercises and lifestyle change and use of acupuncture and herbal medicines. Naturopathic treatment can be used adjunctively with current medical treatment; results are generally better when naturopathic care is implemented sooner rather than later. View published case studies.
Contact the clinic to arrange an individualized assessment – 905-597-7201.

